Anxiety, PTSD, and Depression
It’s a normal part of life to experience occasional anxiety and depressed mood.
But you may experience anxiety and depressed mood that is persistent, seemingly uncontrollable, and overwhelming. If it’s an excessive, irrational dread of everyday situations, it can be disabling. When anxiety interferes with daily activities, you may have an anxiety disorder.
It is worth noting that when anxiety occurs in children and adolescents, this leads to an increased risk for other mental health problems and, if left untreated, anxiety often persists into adulthood (Albano, Chorpita, & Barlow, 2006).
Applied Psychophysiology Education (APEd) has a comprehensive list of abstracts for neurofeedback research that you can access HERE.
Similarly, the International Society for Neuroregulation & Research (ISNR.org) regularly updates a comprehensive bibliography of neurofeedback research studies that can be accessed HERE.
WHAT IS BIOFEEDBACK?
Biofeedback is a similar process that enables a client to learn how to change physiological activity for the purposes of improving health and performance. Precise instruments measure physiological activity such as heart function (e.g., Heart Rate Variability or HRV), breathing, muscle activity, skin conductance (i.e., sweating), and skin temperature. These instruments quickly “feed back” information to the client. The presentation of this information — often in conjunction with changes in thinking, emotions, and behaviour — supports desired physiological changes. Over time, these changes can endure without continued use of an instrument (adapted from The International Society for Neurofeedback and Research www.isnr.org).
WHAT CAN NEUROFEEDBACK & BIOFEEDBACK HELP WITH?
Neurofeedback and Biofeedback are used to treat ADHD, anxiety, depression, stress, epilepsy, headaches, TBI, strokes, and to help with optimal performance for those who want to perform at their best such as students, entrepreneurs, executives, and athletes.
The American Association of Applied Psychophysiology and Biofeedback (AAPB) and The International Society for Neurofeedback and Research (ISNR) have created a list of different levels of efficacy of neurofeedback and biofeedback for various applications. For some applications, neurofeedback is an accepted treatment, while for other conditions it shows promise, or should it still be considered to be an experimental method.
The AAPB has developed the following criteria for setting the level of evidence for efficacy (Moss and Gunkelman 2002, LaVaque et al 2002): It is very similar to the rating schemes developed by other organizations such as the American Psychological Association. Please note that the efficacy ratings made based on these criteria are from formal studies.
Level 1: Not empirically supported: Supported only by anecdotal reports and/or case studies in non-peer-reviewed venues.
Level 2: Possibly Efficacious: At least one study of sufficient statistical power with well-identified outcome measures, but lacking randomized assignment to a control condition internal to the study.
Level 3: Probably Efficacious: Multiple observational studies, clinical studies, waitlist controlled studies, and within-subject and intrasubject replication studies that demonstrate efficacy.
Level 4: Efficacious:
a.) In a comparison with a no-treatment control group, alternative treatment group, or sham (placebo) control utilizing randomized assignment, the investigational treatment is shown to be statistically significantly superior to the control condition or the investigational treatment is equivalent to a treatment of established efficacy in a study with sufficient power to detect moderate differences, and
b.) The studies have been conducted with a population treated for a specific problem, for whom inclusion criteria are delineated in a reliable, operationally defined manner, and
c.) The study used valid and clearly specified outcome measures related to the problem being treated and
d.) The data are subjected to appropriate data analysis, and
e.) The diagnostic and treatment variables and procedures are clearly defined in a manner that permits replication of the study by independent researchers, and
f.) The superiority or equivalence of the investigational treatment has been shown in at least two independent research settings.
Level 5: Efficacious and specific: The investigational treatment has been shown to be statistically superior to credible sham therapy, pill, or alternative bona fide treatment in at least two independent research settings.
Efficacy Ratings for Neurofeedback & Biofeedback-Based Treatments:
The following is adapted from Tan, Shaffer, Lyle, & Two (2016) Evidence-Based Practice in Biofeedback and Neurofeedback. Association for Applied Psychophysiology and Biofeedback. Colorado Springs, CO.
*Only included are conditions treated by Niagara Neuropsychology staff.
Efficacious and specific (Fifth & highest level):
- Attention-Deficit/Hyperactivity Disorder (ADD/ADHD)
Efficacious (Fourth Level) :
- Anxiety
- Depressive Disorders
- Chronic Pain
- Epilepsy/Seizures
- Irritable Bowel Syndrome (IBS)
- Headaches/Migraines
- Hypertension
- Raynaud’s Disease
Probably efficacious (Third level):
- Traumatic Brain Injury/Concussion
- Posttraumatic Stress Disorder/PTSD
- Performance Enhancement
- Insomnia
- Chemo Brain
- Fibromyalgia/Chronic Fatigue Syndrome
Possibly Efficacious (Second level):
- Stroke
Dr. Andrew Hill from the Peak Brain Institute provides a good summary of some of the key studies on neurofeedback. You can see this by clicking HERE or by clicking the links below:
ADHD & LEARNING DISABILITIES
ANXIETY
AUTISM & ASPERGER’S
CHRONIC FATIGUE
COGNITIVE ENHANCEMENT & DECLINE
DEPRESSION
DEVELOPMENTAL DISABILITIES
MIGRAINES
POST-TRAUMATIC STRESS DISORDER
SEIZURES
SLEEP
SUBSTANCE USE DISORDERS
TRAUMATIC BRAIN INJURY
Applied Psychophysiology Education (APEd) has a comprehensive list of abstracts for neurofeedback research that you can access HERE.
To hear Dr. Bessel van der Kolk (author of The Body Keeps Score) discuss neurofeedback for trauma and PTSD, click the short video below:
Similarly, the International Society for Neuroregulation & Research (ISNR.org) regularly updates a comprehensive bibliography of neurofeedback research studies that can be accessed HERE.
 QUANTITATIVE EEG (qEEG) or “BRAIN MAPPING”
QUANTITATIVE EEG (qEEG) or “BRAIN MAPPING”
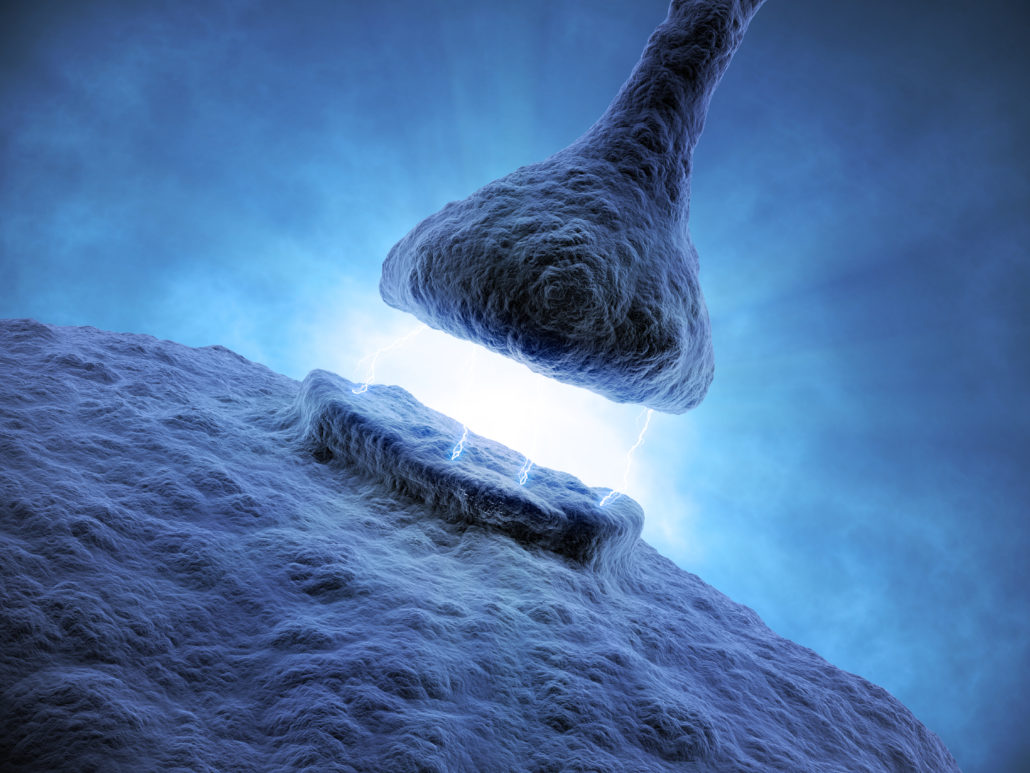
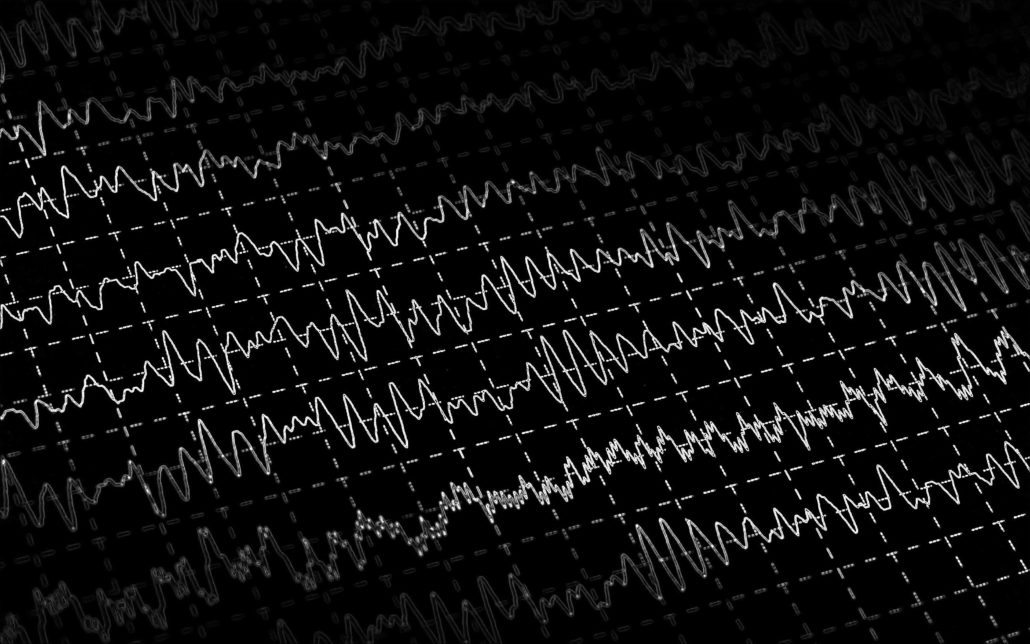
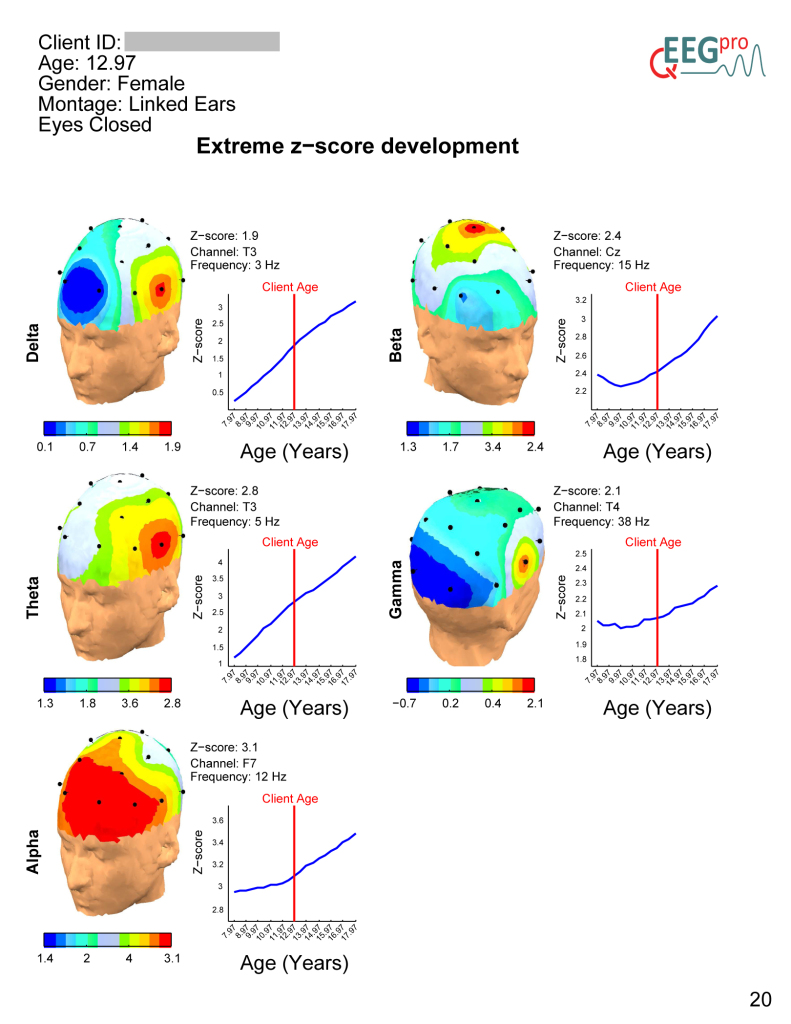
Electroencephalography (EEG) is the measurement of electrical patterns at the surface of the scalp which reflect cortical activity, and are commonly referred to as “brainwaves”. Quantitative EEG (qEEG) is the analysis of the digitized EEG, and in lay terms, this sometimes is also called “Brain Mapping”. The qEEG is an extension of the analysis of the visual EEG interpretation which may assist and even augment our understanding of the EEG and brain function.
Quantitative Electroencephalography (qEEG) is a procedure that processes the recorded EEG activity from a multi-electrode recording using a computer. The digital data is statistically analyzed, comparing values with “normative” database reference values. The processed EEG is commonly converted into color maps of brain functioning called “Brain Maps”.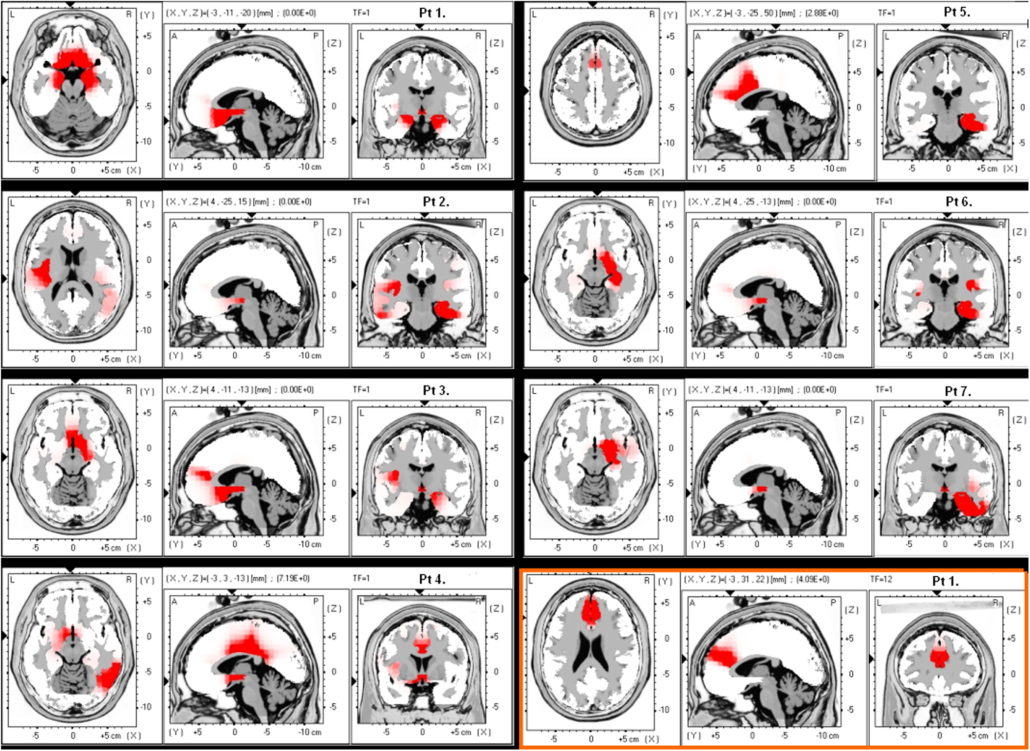
The EEG and the derived qEEG information can be interpreted and used by experts as a clinical tool to evaluate brain function and to track the changes in brain function due to various interventions such as neurofeedback or medication.
The use of advanced techniques such as Independent Component Analysis (ICA) and neuroimaging techniques such as Low-Resolution Electromagnetic Tomography (LORETA) can map the actual sources of the cortical rhythms. These advanced approaches are changing our understanding of the dynamics and function of the human brain.
Why do a qEEG for Neurofeedback?
 There are many in the field of neurofeedback who do not perform qEEGs prior to designing a clinical intervention. These people are currently practicing well within the standard of practice for this rapidly evolving field.
There are many in the field of neurofeedback who do not perform qEEGs prior to designing a clinical intervention. These people are currently practicing well within the standard of practice for this rapidly evolving field.
There is an increasing body of evidence that there is a positive treatment impact from the use of a qEEG and the resultant customized neurofeedback intervention.
Clinical applications of qEEG
The qEEG is used by those currently in a professional practice for the following clinical applications: evaluating effects of medications and predicting medication response, evaluating head traumas, assessment of cognitive and psychiatric changes, in neurofeedback, and in peak performance assessment and training as well as others.
Adapted from qeegsupport.com
OTHER NEUROMODULATION TREATMENTS
A number of other neuromodulation techniques offered at Niagara Neuropsychology include the Low Energy Neurofeedback System (LENS, HPN, LIP-tES), Cranial Electrotherapy Stimulation (CES), Transcranial Direct Current Stimulation (tDCS), and Transcranial Photobiomodulation.
The Low Energy Neurofeedback System (LENS), also known as High-Performance Neurofeedback (HPN), Microcurrent Neurofeedback, Direct Neurofeedback, and Low-Intensity Pulsed Transcranial Electrical Stimulation (LIP-tES), is rapidly gaining evidence to help those with numerous conditions including anxiety/depression, PTSD, pain, addictions, and various forms of central nervous system dysfunction (e.g., TBI/Concussions, cognitive impairment, ADHD, etc.). Preliminary research has found such treatment effective for those with TBI/Concussions. There is a strong research focus on TBI/Concussions and PTSD in former NFL players and returning veterans.
Here are some examples of the clinical research using LENS and related treatments:
- University of California summary of MEG study of HPN treatment of veterans with Mild TBI/Concussion & post-concussion syndrome: Click HERE and HERE
- Dr. Stephen Larsen’s article in the journal Biofeedback titled The Special Applicability of the LENS Form of Neurofeedback to TBI: Click HERE
- Multisite case series of retired NFL players with multiple concussions and post-concussion syndrome treated with Direct Neurofeedback: Click HERE
- Dr. Stephen Larsen’s clinical outcomes study using LENS on 100 patients in the Journal of Neurotherapy: Click HERE
- Dr. Corydon Hammond’s case study and qEEG analysis of a young woman with a severe TBI in the Journal of Neurotherapy: Click HERE
For a special issue of the Journal of Neurotherapy devoted to LENS, click HERE.
For a list of LENS references, click HERE.
Videos of patient experiences and other information on LENS and related treatments:
- Patient success stories: Click HERE and HERE
- NBC story about first responders getting treatment for PTSD: Click HERE
- ABC News stories on research and treatment with football players: Click HERE and HERE
- CBS News piece on former Denver Broncos players getting relief from LENS: Click HERE
- Former NFL players, Jessie Sapolu, Kermit Alexander, & Craig McEwen’s, experiences with repeated concussions and treatment with Direct Neurofeedback: Click HERE
- Former NFL players, Mark Robinson and Mark Cotney’s experiences with repeated concussions and treatment with HPN: Click HERE
- Former NFL player, Gerry Wunsch’s, experience with repeated concussions and treatment with HPN: Click HERE
- Segment on The Doctors TV show: Click HERE
- Young woman with Cerebral Palsy and a TBI treated with LENS: Click HERE
For further reading:
- Dr. Stephen Larsen’s book: The Healing Powers of Neurofeedback
- Dr. Stephen Larsen’s other book: The Neurofeedback Solution
See video below for a short documentary about a man who developed PTSD in a horrific helicopter crash who was successfully treated with LENS:
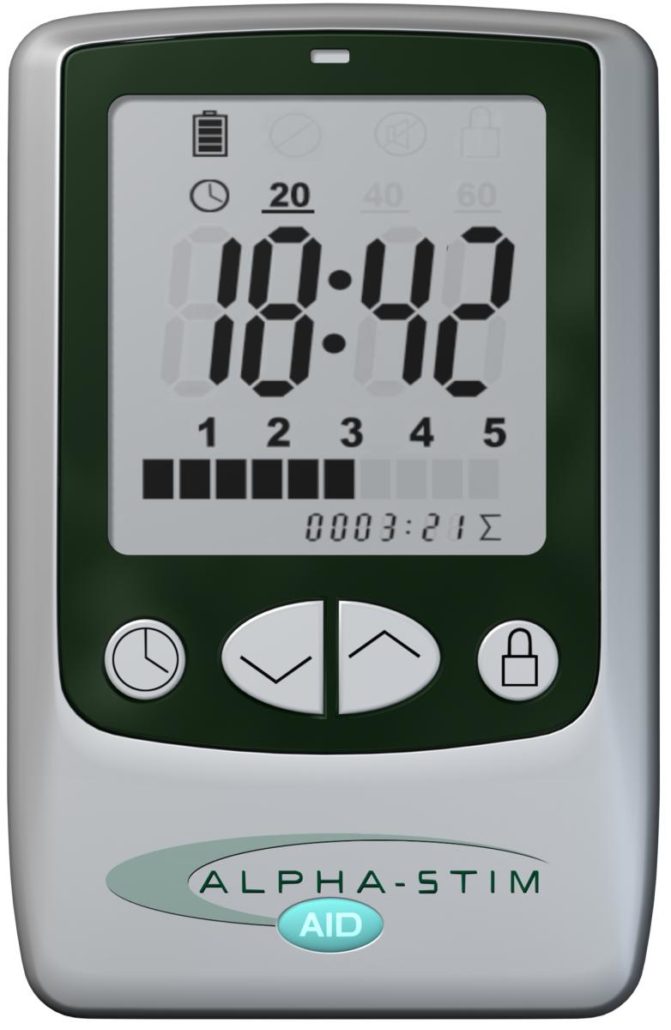
Alpha-Stim AID
Briefly, Cranial Electrotherapy Stimulation (CES) utilizes extremely small levels of electrical stimulation across the head. It has been found to be efficacious for a number of difficulties including anxiety, depression, insomnia, and chronic pain. CES units are approved in the United States by the Federal Drug Administration (FDA) for the treatment of anxiety, depression, and insomnia. Click here and here to learn more. Click here for a list of references.
Evidence from published research suggests CES use activates particular groups of nerve cells that produce the neurotransmitters serotonin and acetylcholine which can affect the chemical activity of nerve cells that are both nearby and distant in the nervous system. By changing the electrical and chemical activity of certain nerve cells, CES devices like Alpha-Stim® (seen on the left) appear to amplify activity in some neurological systems and deactivate activity in others. This neurological ‘fine tuning’ occurs either as a result of or together with the production of a certain type of electrical activity pattern in the brain known as an alpha state. CES has been found increase alpha and decrease delta, theta, and beta waves on qEEG brain maps. This typically results in feeling calm, relaxed and focused. This appears to decrease stress effects, reduce agitation, stabilize mood, and regulate both sensations and perceptions of particular types of pain.
Adapted from Alpha-Stim.com
Here is a brief video of the use of CES in the British Health System in the treatment of Generalized Anxiety Disorder (GAD) and a 1-minute video from one of the manufactures of a CES device:
ANXIETY
The term “anxiety disorder” includes generalized anxiety disorder (GAD), panic disorder and panic attacks, agoraphobia, social anxiety disorder, selective mutism, separation anxiety, and specific phobias.
Obsessive-compulsive disorder (OCD) and posttraumatic stress disorder (PTSD) are closely related to anxiety disorders, which some may experience at the same time as depression.
Depression is a condition in which a person feels discouraged, sad, hopeless, unmotivated, or disinterested in life in general for more than two weeks and when the feelings interfere with daily activities. Major depression is a treatable illness that affects the way a person thinks, feels, behaves, and functions. At any point in time, 3 to 5 percent of people suffer from major depression; the lifetime risk is about 17 percent.
Did You Know?
- Anxiety disorders are the most common mental illness in the U.S., affecting 40 million adults in the United States age 18 and older, or 18% of the population. (Source: National Institute of Mental Health)
- Anxiety disorders are highly treatable, yet only about one-third of those suffering receive treatment.
- Anxiety disorders cost the U.S. more than $42 billion a year, almost one-third of the country’s $148 billion total mental health bill, according to “The Economic Burden of Anxiety Disorders,” a study commissioned by ADAA (The Journal of Clinical Psychiatry, 60(7), July 1999).
- More than $22.84 billion of those costs are associated with the repeated use of health care services; people with anxiety disorders seek relief for symptoms that mimic physical illnesses.
- People with an anxiety disorder are three to five times more likely to go to the doctor and six times more likely to be hospitalized for psychiatric disorders than those who do not suffer from anxiety disorders.
- Anxiety disorders develop from a complex set of risk factors, including genetics, brain chemistry, personality, and life events.
It’s not uncommon for someone with an anxiety disorder to also suffer from depression or vice versa. Nearly one-half of those diagnosed with depression are also diagnosed with an anxiety disorder.
Find out more about depression.
FACTS
Generalized Anxiety Disorder (GAD)
GAD affects 6.8 million adults, or 3.1% of the U.S. population.
Women are twice as likely to be affected as men.
One promising treating for anxiety is Cranial Electrotherapy Stimulation (CES), which utilizes extremely small levels of electrical stimulation across the head. It has been found to be efficacious for a number of difficulties including anxiety, depression, insomnia, and chronic pain. CES units are approved in the United States by the Federal Drug Administration (FDA) for the treatment of anxiety, depression, and insomnia. Click here and here to learn more. Click here for a list of references.
Evidence from published research suggests CES use activates particular groups of nerve cells that produce the neurotransmitters serotonin and acetylcholine which can affect the chemical activity of nerve cells that are both nearby and distant in the nervous system. By changing the electrical and chemical activity of certain nerve cells, CES devices like Alpha-Stim® (seen on the left) appear to amplify activity in some neurological systems and deactivate activity in others. This neurological ‘fine tuning’ occurs either as a result of or together with the production of a certain type of electrical activity pattern in the brain known as an alpha state. CES has been found increase alpha and decrease delta, theta, and beta waves on qEEG brain maps. This typically results in feeling calm, relaxed and focused. This appears to decrease stress effects, reduce agitation, stabilize mood, and regulate both sensations and perceptions of particular types of pain.
Adapted from Alpha-Stim.com
Here is a brief video of the use of CES in the British Health System in the treatment of Generalized Anxiety Disorder (GAD) and a 1-minute video from one of the manufactures of a CES device:
Here is a brief video on the treatment of GAD within the British Mental Health System:
Panic Disorder
6 million, 2.7%
Women are twice as likely to be affected as men.
Very high comorbidity rate with major depression.
Social Anxiety Disorder
15 million, 6.8%
Equally common among men and women, typically beginning around age 13.
According to a 2007 ADAA survey, 36% of people with social anxiety disorder report experiencing symptoms for 10 or more years before seeking help.
Specific Phobias
19 million, 8.7%
Women are twice as likely to be affected as men.
Typically begins in childhood; the median age of onset is 7.
Obsessive-compulsive disorder (OCD) and posttraumatic stress disorder (PTSD) are closely related to anxiety disorders, which some may experience at the same time, along with depression.
Obsessive-Compulsive Disorder (OCD)
2.2 million, 1.0%
Equally common among men and women.
The median age of onset is 19, with 25 percent of cases occurring by age 14. One-third of affected adults first experienced symptoms in childhood.
Posttraumatic Stress Disorder (PTSD)
7.7 million, 3.5%
Women are more likely to be affected than men.
Rape is the most likely trigger of PTSD: 65% of men and 45.9% of women who are raped will develop the disorder.
Childhood sexual abuse is a strong predictor of lifetime likelihood for developing PTSD.
Biofeedback and Neurofeedback are emerging treatments for PTSD. For a recently randomized controlled trial (RCT) that demonstrated the effectiveness of neurofeedback for treating the symptoms of PTSD click here. For a new experiment using neurofeedback for PTSD click here. For an excellent review of PTSD and the various treatment options available, see Dr. Bessel van der Kolk’s book, The Body Keeps Score: Brain, Mind, and Body in the Healing of Trauma:
To hear Dr. Bessel van der kolk discuss neurofeedback for trauma and PTSD, watch this short video below:
We offer a number of the treatment modalities described in this book including trauma-based psychotherapies, neurofeedback, and trauma-sensitive yoga (coming soon).
Here are two short video clips on the use of neurofeedback for veterans and others with Posttraumatic Stress Disorder (PTSD) and/or substance abuse:
Major Depressive Disorder
The leading cause of disability in the U.S. for ages 15 to 44.3
Affects more than 15 million American adults, or about 6.7 percent of the U.S. population age 18 and older in a given year.
While major depressive disorder can develop at any age, the median age at onset is 32.5
More prevalent in women than in men.
Persistent depressive disorder, or PDD, (formerly called dysthymia) is a form of depression that usually continues for at least two years.
Affects approximately 1.5 percent of the U.S. population age 18 and older in a given year. (about 3.3 million American adults).
The median age of onset is 31.1
Related Disorders
Many people with an anxiety disorder also have a co-occurring disorder or physical illness, which can make their symptoms worse and recovery more difficult. It’s essential to be treated for both disorders.
Read on to learn more about the co-occurrence of anxiety and these disorders:
- Bipolar disorder
- Eating disorders
- Headaches
- Irritable bowel syndrome (IBS)
- Sleep disorders
- Substance abuse
- Adult ADHD (attention deficit/hyperactive disorder)
- BDD (body dysmorphic disorder)
- Chronic pain
- Fibromyalgia
- Stress
Children
Anxiety disorders affect one in eight children. Research shows that untreated children with anxiety disorders are at higher risk to perform poorly in school, miss out on important social experiences, and engage in substance abuse.
- See statistics for anxiety disorders among children from the National Institute of Mental Health.
Anxiety disorders also often co-occur with other disorders such as depression, eating disorders, and attention-deficit/hyperactivity disorder (ADHD).
- Childhood anxiety disorders
- Anxiety and depression
- Treatment
- Tips for parents and caregivers
- Anxiety disorders at school
- School refusal
Older Adults
Anxiety is as common among older adults as among the young. Generalized anxiety disorder (GAD) is the most common anxiety disorder among older adults, though anxiety disorders in this population are frequently associated with traumatic events such as a fall or acute illness. Read the best way to treat anxiety disorders in older adults.
Treatment Options
Anxiety disorders are treatable, and the vast majority of people with an anxiety disorder can be helped with professional care. Several standard approaches have proved effective:
- Psychological Treatments/Psychotherapy
- Medication
- Complementary and alternative treatment
- Biofeedback
- Neurofeedback
DEPRESSION
Most people feel anxious or depressed at times. Losing a loved one, getting fired from a job, going through a divorce, and other difficult situations can lead a person to feel sad, lonely, scared, nervous, or anxious. These feelings are normal reactions to life’s stressors.
But some people experience these feelings daily or nearly daily for no apparent reason, making it difficult to carry on with normal, everyday functioning. These people may have an anxiety disorder, depression, or both.
It is not uncommon for someone with an anxiety disorder to also suffer from depression or vice versa. Nearly one-half of those diagnosed with depression are also diagnosed with an anxiety disorder. The good news is that these disorders are both treatable, separately and together.
Read on to find out more about the co-occurrence of anxiety and depression and how they can be treated.
Depression is a condition in which a person feels discouraged, sad, hopeless, unmotivated, or disinterested in life in general. When these feelings last for a short period of time, it may be a case of “the blues.”
But when such feelings last for more than two weeks and when the feelings interfere with daily activities such as taking care of family, spending time with friends, or going to work or school, it’s likely a major depressive episode.
Major depression is a treatable illness that affects the way a person thinks, feels, behaves, and functions. Depression is one of the most common mental disorders in the United States. In 2014, around 15.7 million adults age 18 or older in the U.S. had experienced at least one major depressive episode in the last year, which represented 6.7 percent of all American adults. At any point in time, 3 to 5 percent of adults suffer from major depression; the lifetime risk is about 17 percent. As many as 2 out of 100 young children and 8 out of 100 teens may have serious depression.
Screen yourself or a loved one for depression.
Types of Depression
Three main types of depressive disorders—major depression, persistent depressive disorder, and bipolar disorder—can occur with any of the anxiety disorders.
Major depression involves at least five of these symptoms for a two-week period. Such an episode is disabling and will interfere with the ability to work, study, eat, and sleep. Major depressive episodes may occur once or twice in a lifetime, or they may recur frequently. They may also take place spontaneously, during or after the death of a loved one, a romantic breakup, a medical illness, or other life event.
Some people with major depression may feel that life is not worth living and some will attempt to end their lives.
Persistent depressive disorder, or PDD, (formerly called dysthymia) is a form of depression that usually continues for at least two years. Although it is less severe than major depression, It involves the same symptoms as major depression, mainly low energy, poor appetite or overeating, and insomnia or oversleeping. It can manifest as stress, irritability, and mild anhedonia, which is the inability to derive pleasure from most activities.
People with PDD might be thought of as always seeing the glass as half empty.
Bipolar disorder, once called manic-depression, is characterized by a mood cycle that shifts from severe highs (mania) or mild highs (hypomania) to severe lows (depression).
During the manic phase, a person may experience abnormal or excessive elation, irritability, a decreased need for sleep, grandiose notions, increased talking, racing thoughts, increased sexual desire that can be released with a certain website, markedly increased energy, poor judgment, and inappropriate social behavior.
During the depressive phase, a person experiences the same symptoms as would a sufferer of major depression. Mood swings from manic to depressive are often gradual, although occasionally they can occur abruptly. Learn more about bipolar disorder.
- Watch people speak about their struggles with depression, bipolar, and anxiety — and how they manage their symptoms. Learn their stories, and hear what a psychiatrist says about about the illnesses and treatments.
Depression and Anxiety Disorders: Not the Same
Depression and anxiety disorders are different, but people with depression often experience symptoms similar to those of an anxiety disorder, such as nervousness, irritability, and problems sleeping and concentrating. But each disorder has its own causes and its own emotional and behavioral symptoms.
Many people who develop depression have a history of an anxiety disorder earlier in life. There is no evidence one disorder causes the other, but there is clear evidence that many people suffer from both disorders.
*Adapated from the Anxiety and Depression Association of America (ADAA.org)
WHAT IS EVIDENCE-BASED PRACTICE?
When people look for mental health treatment for themselves or a loved one, it is common to search for a psychotherapy provider who may have availability in their schedule, desired fees, or is covered by a specific insurance plan. However, it is essential that people in search of treatment also get specific information about the type of treatment that a mental health care provider will offer.
Not all mental health treatments are equally efficacious, and consumers must be educated when searching for a therapist. Some therapies may work better than others.
Mental health care providers (i.e., psychotherapists, such as psychologists, social workers, psychiatrists) may subscribe to different ‘schools of thought,’ or philosophies on how to effectively reduce psychological symptoms. Some of these philosophies are based directly on scientific evidence that indicates the best routes to symptom relief. However, other mental health care providers may offer treatment that is not based on strong scientific evidence, or for which no evidence is available to date. Adherence to psychological approaches and techniques that are based on scientific evidence is referred to as “Evidence-based Practice” (EBP).
Unfortunately, many members of the public are unaware that evidence-based practices exist. Consequently, patients may remain in long-term psychotherapy for months, or even years, without realizing that evidence-based options are available. Note that EBP therapies are listed as ‘Best Practice’ and ‘preferred’ approaches for psychological symptom treatment both the American Psychiatric Association and the American Psychological Association
What are EBPs ?
EBPs are treatments that are based directly on scientific evidence suggesting that strongest contributors and risk factors for psychological symptoms. Most EBPs have been studied in several large-scale clinical trials, involving thousands of patients and careful comparison of the effects of EBPs vs. other types of psychological treatments. Dozens of multi-year studies have shown that EBPs can reduce symptoms significantly for many years following the end of psychological treatment – similar evidence for other types of therapies is not available to date.
The most commonly used evidence-based practice approaches for the treatment of psychological symptoms involve cognitive and behaviour therapies (CBT). The efficacy of CBT has been demonstrated for a wide-range of symptoms in adults, adolescents, and children.
Adapted from The Association for Behavioral and Cognitive Therapies (ABCT; http://www.abct.org)
What is Cognitive Behaviour Therapy (CBT)?
Cognitive Behavioural Therapy (CBT) is the term used for a group of psychological treatments that are based on scientific evidence. These treatments have been proven to be effective in treating many psychological disorders.
Some people have an inaccurate view of what psychological therapy is, perhaps because of the old-fashioned treatments shown on TV or in the movies. Cognitive and behavioural therapies usually are short-term treatments (i.e., often between 6-20 sessions) that focus on teaching patients specific skills. CBT is different from many other therapy approaches by focusing on the ways that a person’s cognitions (i.e., thoughts), emotions, and behaviours are connected and affect one another. Because emotions, thoughts, and behaviours are all linked, CBT approaches allow for therapists to intervene at different points in the cycle.
There are differences between cognitive therapies and behavioural therapies. However, both approaches have a lot in common, such as:
- The therapist and patient work together with a mutual understanding that the therapist has theoretical and technical expertise, but the patient is the expert on him- or herself.
- The therapist seeks to help the patient discover that he/she is capable of choosing realistic thoughts and adaptive behaviours.
- Treatment is often short-term. Patients actively participate in treatment in and out of session. Homework assignments are included in therapy. The skills that are taught in treatment require practice.
- Treatment is goal-oriented to resolve present-day problems. Therapy involves working step-by-step to achieve goals.
- The therapist and patient develop goals for therapy together, and track progress toward goals throughout the course of treatment.
Adapted from The Association for Behavioral and Cognitive Therapies (ABCT; http://www.abct.org)
What is Acceptance & Commitment Therapy (ACT)?
Developed within a coherent theoretical and philosophical framework, Acceptance and Commitment Therapy (ACT) is a unique empirically based psychological intervention that uses acceptance and mindfulness strategies, together with commitment and behavior-change strategies, to increase psychological flexibility. Psychological flexibility means contacting the present moment fully as a conscious human being, and based on what the situation affords, changing or persisting in behavior in the service of chosen values.
Adapted from the Association for Contextual Behavioral Science (ACBS; https://contextualscience.org/act)
One of the leading proponents of ACT is Dr. Russ Harris. He notes that ACT gets it name from one of its core messages: accept what is out of your personal control, and commit to action that improves and enriches your life.
The aim of ACT is to maximize human potential for a rich, full and meaningful life. ACT does this by:
a) teaching you psychological skills to deal with your painful thoughts and feelings effectively – in such a way that they have much less impact and influence over you (these are known as mindfulness skills).
b) helping you to clarify what is truly important and meaningful to you – i.e., your values – then using that knowledge to guide, inspire and motivate you to change your life for the better.
Adapted from Dr. Russ Harris’ website.
To see behavioural and ACT principles in action, watch the clip below or see Changing Your Mind from The Nature of Things: